It’s that special time of year, folks!
Yes, step right up ladies and gentlemen, and welcome to the
2014 Annual Red Meat Causes Cancer Wankfest!
Never heard of the ARMCCW, you say? No idea what it involves?
Well, let me tell you all about it, then.
Every year, the deluded sods that largely comprise the nutritional epidemiology community partake in a ritual where they
“associate”
red meat with cancer incidence. Sometimes it’s overall cancer, other
times they zero in on a particular malignancy such as colon, rectal,
prostate, or pancreatic cancer.
Sometimes, they get a wee bit depressed by the whole cancer thing, so instead temporarily try their hand at
“associating”
read meat with heart disease. But cancer is where the real action is at
when it comes to bashing red meat, so that’s where the epidemiological
shysters tend to focus their energy.
Before we learn which cancer is the star of 2014’s ARMCCW, let’s take
a quick look behind the scenes to see exactly how this farce operates.
The Sham, and How It Works
I’ve written about this appalling charade before
here and
here, so long-time readers probably already know where this is heading. And so I’ll try to be brief(ish).
Basically, epidemiologists dredge large confounder-prone prospective
studies, jump all over a pathetically weak statistical association
between meat and their malignancy of choice, then carry on like it’s
causal.
It’s a prolific scam, because they can always count on red meat to show an association with cancer risk.
Not because red meat is carcinogenic. Unless you regularly consume
charred or overcooked red meat, it isn’t. Red meat, in fact, is the
healthiest, most nutrient-dense food known to mankind. That’s why our
ancestors often placed themselves in great physical danger to get at it.
What, you think they would’ve risked life and limb to get fresh red
meat if their nutritional needs could’ve been met by wild spinach and
acorns?
Yeah, right. Only vegetarians believe absurd shit like that.
So why, then, would meat ever be associated with cancer in these epidemiological studies?
Because, invariably, people who eat the most red meat in these
studies also have the highest rate of truly unhealthy behaviours like
smoking, low physical activity, excess alcohol consumption, excess
caloric consumption, and on and on and on.
Why would people who eat the most red meat exhibit poorer overall health practices?
Because people who care less about their health don’t just ignore perfectly sensible health messages like
“Don’t Smoke”,
“Do Regular Exercise” and
“Eat Your Veggies”. They also ignore patently idiotic health messages with no foundation in reality, such as
“Avoid Red Meat”!
And so people who smoke more, exercise less, hit the booze more
often, eat a poorer diet overall, have a higher bodyweight, etc, etc,
also tend to eat more red meat.
These people, not surprisingly, will be at higher risk of cancer. And so red meat becomes guilty by association.
If the nutritional epidemiologists responsible for these studies
weren’t so deluded, they’d stop right there, and admit their work
provides nothing but statistical associations of unknown origin. To
establish the origin of those associations as causal, they’d need to
conduct randomized clinical trials comparing groups of subjects randomly
assigned to diets containing red meat, or to diets not containing red
meat.
They’d let these trials run for a good stretch of time, then at the
end tally up the number of people who got cancer in each dietary group.
If the red meat group had a significantly higher incidence of cancer
during the trial, then we’d have pretty strong grounds for believing red
meat causes cancer. Of course, we’d need follow-up RCTs to replicate
these results and confirm they weren’t just a “fluke” finding.
But epidemiologists don’t like RCTs, and here’s why:
–The results of quality RCTs have an annoying habit of showing
epidemiological findings to be utter bollocks. An excellent example of
this is the
“Whole-Grains are Good for You!” sham.
Epidemiological studies supporting this terribly mistaken notion are a
dime a dozen, but every time an RCT (both the parallel arm and crossover
variety) has examined this issue, the whole-grain group has fared
worse. Because that flies in the face of all the
“healthy whole-grain”
propaganda that we’ve been bombarded with by health ‘experts’ and
‘authorities’, those ‘experts’ and ‘authorities’ do what most people
heavily vested in a false belief do:
Evade reality.
They simply pretend the RCTs don’t exist, and completely ignore them
when writing and talking about the issue. Instead, they enthusiastically
cite all the epidemiological studies showing an
“association”
between whole grain cereals and reduced disease risk (I’ve discussed
this disgraceful phenomenon thoroughly but concisely in my most recent
book
Whole Grains, Empty Promises).
–RCTs are expensive, and they involve a lot of work. And even the
best RCTs are usually only good for a handful of journal articles.
Epidemiological studies, on the other hand, are like popular prime time
soap operas and reality shows: A lucrative, never ending bounty of
bullshit.
In epidemiological studies, you don’t need to randomize people, you
don’t need to give them detailed instruction, and you don’t need to take
any measures to encourage or monitor compliance with any intervention.
Shit, you don’t even need an intervention!
In an epidemiological study, you simply recruit a bunch of people,
give them a questionnaire at the start and, if you can be assed, a
follow-up survey every few years.
When the forms come back in the mail, you fire up the computer, run some data analyses and – bingo! – you’ve got a paper!
Or, more likely, you’ll have twenty papers. Or if you’re from the
Harvard Public School of Health, you’ll eventually have dozens upon
dozens of papers from the one study!
Because they’re far less sophisticated and hence easier to conduct,
epidemiological studies can involve far larger numbers of subjects. In a
world where B-I-G things – be they incomes, buildings, boats, or boobs –
tend to impress more people, studies involving tens of thousands and
sometimes hundreds of thousands of subjects have a giddying effect on
researchers and journalists.
Also, because there’s no intervention, you aren’t forced to focus on a
specific health issue, which is the case with an RCT. You can’t, for
example, conduct an RCT testing the effect of red meat intake on cancer,
then use the data from that RCT to also publish a paper on the effect
of blueberry intake on haemorrhoid incidence. The design of the study
just won’t allow it.
But you can do exactly that with an epidemiological study in which
you have intake data for dozens of foods and questionnaires that ask
about the incidence of a whole host of health ailments. Never mind that
this intake data is self-reported and therefore well-established to be
of highly dubious quality – epidemiologists certainly don’t. They just
go ahead and take it seriously, crunch the numbers, and spit out papers
one after the other.
For researchers and academics, there’s a lot of prestige attached to
being a prolific author of published, peer-reviewed papers. The more the
merrier. And a large nutritional epidemiological study offers a
limitless opportunity for the researchers involved to accumulate
published titles to their names. Don’t believe me? Fine, enter the
following into Pubmed and see what happens:
“Nurses’ Health Study”, “Harvard Physicians’ Study”, “Framingham Study”, “INTERHEART” …
It’s the old quantity versus quality scenario in full effect. RCTs
might be considered the gold standard of scientific research, but we
live in a world where fiat currencies rule the roost. And like the fifty
dollar note in your pocket that is nothing but ink on a bit of paper
(actual worth of ink + paper = a few cents), all is not what it seems
with epidemiology.
The 2014 Wankfest
ARMCCW 2014 involves the
Nurses’ Health Study II, emanating from Ground Zero of epdemi-hogwash: The Harvard School of Public Health.
It’s a hallowed place, Harvard. Which, sadly, gives the nonsense
emanating from their nutritional epidemiologists a veneer of prestige
and respectability. But make no mistake: Underneath that smart-looking
polished mahogany exterior lies the same old confounder-prone rot.
Soooo … what cancer is taking centre stage at this year’s ARMCCW?
Breast cancer.
The researchers claim
“each serving per day increase in red meat was associated with a 13% increase in risk of breast cancer.”
They further claim:
“When this relatively small relative risk is applied to breast
cancer, which has a high lifetime incidence, the absolute number of
excess cases attributable to red meat intake would be substantial, and
hence a public health concern. Moreover, higher consumption of poultry
was related to a lower incidence of breast cancer in postmenopausal
women. Consistent with the American Cancer Society guidelines,
replacement of unprocessed and processed red meat with legumes and
poultry during early adulthood may help to decrease the risk of breast
cancer.”
What this shows is that, even if you work at The World’s Most
Prestigious University!™, you can still be utterly clueless about
scientific reality. Modern humans have constructed a societal structure
in which bullshit can flourish and wield great influence, and
nutritional epidemiology thrives as a result.
Before I explain in more detail why the association between red meat
and breast cancer doesn’t even begin to qualify as causal, I’d like to
address the observation that
“higher consumption of poultry was related to a lower incidence of breast cancer in postmenopausal women.”
This is hardly the first epidemiological study to notice that poultry and/or fish are
“associated” with improved health outcomes.
Why?
For the very same reason that red meat is
“associated” with
poorer outcomes: Health conscious individuals who smoke less, exercise
more, don’t binge drink etc, etc, etc are more likely to eat white meat
instead of red. Because that’s what all the public health messages and
poncey “wellness” magazines they read tell them to do.
Anyway, let’s look at the
study itself.
It involved 88,803 premenopausal women from the Nurses’ Health Study II who completed a “semi-quantitative” food frequency
questionnaire
in 1991, 1995, 1999, 2003, and 2007 asking about usual dietary intake
and alcohol consumption for the previous 12 months. The researchers also
asked about things like weight, family history of breast cancer,
smoking, race, age at menarche, parity (ie, number of children they’d
given birth to), and oral contraceptive use.
They followed the women for an average of 20 years, during which time 2,830 cases of breast cancer were documented.
When carrying out their pre-determined task of linking red meat to
cancer risk, the researchers divided the women up into 5 categories
according to their red meat consumption. And sure enough, as red meat
consumption went up, so too did breast cancer risk.
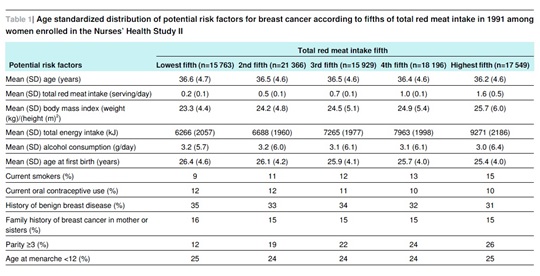
But take a look at Table 1 from the study below:
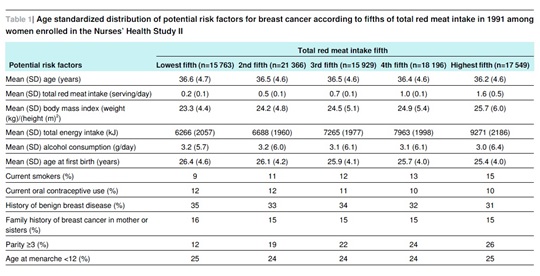
You can see that as red meat consumption went up, the number of smokers
also went up in a perfect linear fashion. The group with the highest red
meat intake had 67% more smokers.
Gee, you think that might increase their breast cancer risk?
Naaaah…
Now, if smoking went up in step with red meat consumption, you’d
expect other unhealthy behaviours including physical inactivity, junk
food consumption, recreational drug use, and erratic sleep habits to
increase along with red meat consumption. Despite their overwhelming
importance, the researchers didn’t see fit to ask about and/or include
these variables in Table 1.
But we do know as red meat intake rose, so too did total caloric consumption and BMI.
But that’s not all. Take a look at the second last line, the one that begins with “
Parity ≥3 (%)“.
The figures that follow are the percentage of women in each group who
reported giving birth to 3 or more children. Again, as red meat intake
goes up, so too does the number of women reporting having 3 or more
kids. The difference is quite pronounced – those with the highest red
meat intake were more than twice as likely to have had 3 or more full
term pregnancies.
Why does this matter?
Because parity is an important risk factor for breast cancer. While
giving birth to one’s first child at a young age has been consistently
associated with a lower risk of late onset cancer, the risk of early
onset cancer (i.e. the type of cancer that would be more likely to occur
during a study like this)
rises with each and every pregnancy a woman has.
I won’t go into the physiological reasons for this – if you’re
interested consult Dr Google and you’ll find plenty of information. All I
will point out here is the bleeding obvious: The number of children a
woman bears has little if anything to do with the amount of red meat she
eats and everything to do with the amount of fornication (sans
effective contraception) she engages in when ovulating.
Fucking duh (evidently, the epidemiologists at The World’s Most
Prestigious University!™ need a little more basic sex education).
But again, blaming clearly established risk factors like smoking and
higher parity for breast cancer doesn’t sit too well with the anti-red
meat agenda. Yep, this is the Blame Red Meat Wankfest, gotta get with
the festive spirit!
But how do you do that when starkly contrasting smoking and parity rates threaten to ruin the party?
Easy.
You pull out the favourite prop of epidemiologists all around the world – the statistical wand!
You take this pretty pink little wand, you wave it all about, and when you finish you pretend you have magically
“adjusted” for such pesky confounders as smoking and parity!
The only way you can truly adjust for anything is to take your
subjects and randomly assign them to either an intervention (red meat)
or control (no red meat) group. In other words, you do a randomized
clinical trial (RCT). The randomization process negates the problem that
plagues nutritional epidemiological studies – confounding. That’s
because randomly assigning people to the intervention and control groups
means people with unhealthy habits are just as likely as people with
healthy habits to end up in the no-red meat group. And vice versa.
But as we’ve already seen, epidemiologists hate RCTs. So what they do
instead is engage in an Emperor-has-no-clothes charade where they use
formulas – derived Ponzi-style from other confounder-prone
epidemiological studies – to statistically
“adjust” for confounding variables. They honestly believe they can tease out the effect of these variables
after the fact.
You and I might call this delusional. Epidemiologists call it
“multivariate analysis.”
For a sterling example of how multivariate analysis routinely falls flat on its face, I refer you back to the
“whole-grains are healthy!”
hyperbole. Again, really big epidemiological studies whose crude data
was carefully massaged, uh, I mean, adjusted, show wonderfully lower
rates of morbidity and mortality among those eating the most
whole-grains.
But when the theory is put to the test in randomized clinical trials,
those assigned to eat more whole-grains or cereal fibre (the exact
component of whole-grains we are supposed to believe is wonderfully
healthy) are the ones who suffer higher rates of morbidity and
mortality. Again, if you want a detailed but easy-to-read breakdown of
this phenomenon, grab yourself a copy of
Whole Grains, Empty Promises
(all proceeds support the International Ramone Foundation, a non-profit
organization devoted to keeping my dog happy, well-fed, and built like a
brick outhouse).
Remember, quality (RCTs) versus quantity (epidemiology).
So there it is, folks. Now you know all about the Annual Red Meat
Causes Cancer Wankfest, and how it works. Think of an Olympic Torch, but
one that spouts bullshit instead of flames. It travels the world,
getting handed from one anti-red meat group to another, passing with
unusual frequency through Boston, Massachusetts.
One last thing before I sign off. I’ve actually made this point
before, but because a lot of people are dumb as shit I need to make it
again. I sound like I have a very low opinion of epidemiology and … well
… I do. The amount of utter bullshit that is propped up and made to
look like science as a result of garbage epidemiological studies is
truly astounding. And quite disheartening, when you think of all the
unnecessary misery and mortality that has resulted from totally missing
the boat on what really causes things like cancer and heart disease.
It’s an absolute disgrace.
However, I’m not against
all epidemiology. The link between
cigarette smoking and lung cancer owes much to epidemiology. Ditto with
infectious disease or food poisoning outbreaks – epidemiology allows
researchers to determine key similarities among those afflicted and
track down the source so they can begin containing the problem as
quickly as possible.
It’s when epidemiology turned its attention to dietary intake and
chronic disease that things really turned to crap. Epidemiology is well
suited to situations like those I listed above, because the factors
being studied are so clear cut and the mechanisms so obvious, there’s
far less doubt about the relationship that intertwines them all. For
example, it doesn’t take a brain (or lung) surgeon to realize the
possibility that smoking cigarettes and filling your lungs with noxious
fumes for years on end might cause lung cancer.
Nor do you need to be particularly bright to realize what might be
going on when people all over the country suddenly start showing up at
emergency wards vomiting their guts out, and subsequent investigation
reveals that the one thing they all have in common is that they ate a
particular brand of pre-packaged raw salad, emanating from a single food
processing plant in Boise, Idaho.
But when epidemiology experienced these early successes, developed
way too much of a cocky swagger, and figured it would turn its attention
to the link between diet and chronic disease … that’s the point at
which it crossed the line from utilitarian and helpful and instead
started venturing into downright delusional territory.
Not only are the confounding variables
involved in diet and lifestyle too numerous for any non-omnipotent
creature (i.e. any human researcher) to fully account for, but it’s also
well established that misreporting in dietary questionnaires is not the
exception but the norm.
The continual and unavoidable presence of confounding and
misreporting in population-based studies is why most nutritional
epidemiology is
absolute bullshit.
Don’t base your health decisions on absolute bullshit.
 The favoured drink of epidemiologists worldwide.
The favoured drink of epidemiologists worldwide.
author has no relationship whatsoever with the meat industry – nor any
other food-related industry – aside from that of paying consumer.
—
Anthony Colpo is author of
The Fat Loss Bible, The Great Cholesterol Con and
Whole Grains, Empty Promises.
Copyright © Anthony Colpo.
Disclaimer: All content on this web site is provided for information
and education purposes only. Individuals wishing to make changes to
their dietary, lifestyle, exercise or medication regimens should do so
in conjunction with a competent, knowledgeable and empathetic medical
professional. Anyone who chooses to apply the information on this web
site does so of their own volition and their own risk. The owner and
contributors to this site accept no responsibility or liability
whatsoever for any harm, real or imagined, from the use or dissemination
of information contained on this site. If these conditions are not
agreeable to the reader, he/she is advised to leave this site
immediately.