Ketogenic Diets, I: Ways to Make a Diet Ketogenic
I was going to write a single post about how to implement a therapeutic ketogenic (ketone-generating) diet.
But then I thought it was worth spelling out issues in some detail.
There are various ways to make a diet ketogenic, and different ways are
appropriate in different diseases. Also, different diseases may call for
a different balance between three criteria:
1)
Safety. Does the diet generate side effects?
2)
Therapy. Is the diet as curative as it can be?
3)
Pleasurability and practicality. Is the diet unnecessarily expensive, unpalatable, or boring?
I soon realized that with so many factors affecting diet design, it
would be hard to fit everything into a single post. So I’m going to
split up the discussion into parts. Today I’ll look at the various ways
to make a diet ketogenic. On Tuesday I’ll look at how to design a diet
for Kindy’s NBIA kids. We’ll look at what they’re eating now, and
consider ways they might be able to improve their diets further – and,
hopefully, get further improvements in health, longevity, and function.
Maybe we’ll look at some other diseases after that, or maybe I’ll
just move on to the lemon juice series I’ve been planning. The lemon
juice and acid-base balance issues will fit in nicely since kidney
stones and acidosis are risks of ketogenic diets and lemon juice
relieves those risks.
So: how can we make a diet ketogenic?
What Is a Ketone?
The liver is responsible for making sure that the body (but
especially the brain and heart) have access to a sufficient supply of
energy from the blood. To fulfill that responsibility, it manufactures
two energy substrates – glucose and
ketones – and exports them into the blood as needed.
The most important ketones are
acetoacetic acid and
beta-hydroxybutyric acid.
Ketones are water-soluble small molecules. They diffuse throughout
the body into cells, and are taken up by mitochondria and oxidized for
energy.
Ketones are especially important to neurons, which can only consume
glucose or ketones. So if something is wrong with glucose metabolism,
ketones can be the sole usable energy source of neurons. (Other cell
types, but not neurons, burn fats.)
Manufacture of Glucose and Ketones During Starvation
While preparing this post, I was surprised at how long it took for
doctors to appreciate that ketones are an acceptable alternative energy
source for the brain. The realization that the brain doesn’t perpetually
rely on glucose during starvation apparently didn’t sink in until 1967!
The use of prolonged starvation for the treatment of
obesity has posed a fascinating problem; namely, that man is capable of
fasting for periods of time beyond which he would have utilized all of
his carbohydrate resources and all of his proteins for gluconeogenesis
in order to provide adequate calories as glucose for the central nervous
system.
This study was designed to clarify the apparent paradox, and it was
found that beta-hydroxybutyrate and acetoacetate replace glucose as the
brain’s primary fuel during starvation. [1]
This makes it a bit easier to understand why ketogenic diets have not
yet become standard therapies for neurological diseases. Epileptics
caught a lucky break – the ketogenic diet was already in use for
epilepsy in the 1920s. The ketogenic diet’s therapeutic potential for
other neurological disorders probably couldn’t have been appreciated
until after 1967, and by then medicine had turned its back on dietary
therapy.
But back to ketones. During starvation, glucose and ketones have to
be manufactured from body parts. The body’s resources include:
- Glycogen – a storage form of glucose. However, glycogen supplies are minimal.
- “Complete” protein – a mix of amino acids similar to that found in animal meats.
- Long-chain fats – fatty acids 14-carbons or longer in length,
attached to a glycerol backbone as either triglycerides or
phospholipids.
During starvation, different raw materials end up as different energy substrates:
- Glycogen can be used to make glucose but not ketones. So glycogen converts 100% to glucose.
- Protein is broken down into its constituent amino acids. Some amino
acids can become glucose but never ketones; some can become either; some
can become ketones but glucose. “Complete” protein usually found in the
body typically converts 46% to ketones, 54% to glucose. [UPDATE: Actually, this is incorrect. As Tony Mach points out in the comments,
complete protein converts 20% to ketones, 80% to glucose. The 46-54
ratio is the contribution to Wilder’s ketogenic ratio, see below.]
- Triglycerides and phospholipids are broken up into their constituent
parts. The fatty acids can make ketones but not glucose; the glycerol
backbones can make glucose but not ketones. Typically, 10-12% of energy
from a triglyceride is in the form of glycerol (which has the potential
to become glucose) and 88-90% is in the form of fatty acids (which have
the potential to become ketones).
As we note in the book, during starvation the body is cannibalizing
tissues that are roughly 74% fat, 26% protein by calories. Due to the
preponderance of fat, starvation is highly “ketogenic” (ketone
generating). The 26% of calories that are protein generate roughly equal
amounts of ketones and glucose, but the 74% of calories that are fat
generate only ketones.
This doesn’t mean that during starvation ketones are 87% of energy
and glucose 13% of energy. Most of the fats are burnt directly for
energy without conversion to ketones. But a fair amount of fats are
diverted into ketone production, and ketones are abundant during
starvation.
A Ketogenic Diet Using “Body Part Foods”
If your diet could include only compounds found in the body –
glucose, complete protein, and long-chain fats stored as triglycerides
or phospholipids – then we can use the above numbers to estimate the
“ketogenic potential” of the diet.
I have to credit commenter “Cathy” at the PaNu Forum for this next part. Kindy posted
a question about the ketogenic diet for NBIA on the PaNu Forum in October 2010, and Cathy left an informative comment:
The ketogenic formula was originally developed by Wilder
at the Mayo clinic in the 1920’s. By googling WILDER KETOGENIC FORMULA, I
found a link to the book “The Ketogenic Diet: A Treatment for Epilepsy”
published in 2000. Quite a bit of the book is available for reading
online; here is the URL
.
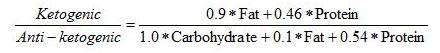
On page 36 of this book is Wilder’s formula for the ketogenic potential of a diet:
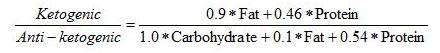
This formula basically treats all fats as triglycerides of long-chain
fatty acids, and protein as “complete” protein with a typical mix of
amino acids. It makes a ratio of the ketone precursors to the glucose
precursors.
Wilder’s “ketogenic ratio” was used by Dr. Richard Bernstein in his
Diabetes Solution
to help people appraise the ketogenicity of a diet. A ratio below 1.5
signifies a minimally ketogenic diet; the higher the ratio goes above
1.5, the more ketones will be generated.
Other Dietary Ketone Precursors
If you’re not starving, you have the opportunity to eat foods that are not components of the body, and that are
more ketogenic than “body part foods.”
Specifically, you can eat:
- Short-chain fats such as are found in coconut oil.
- A mix of amino acids that is not “complete,” but is biased toward the ketogenic amino acids.
If you do this then your diet will be more ketogenic than Wilder’s formula would suggest.
Eating these foods may be advantageous. For instance, suppose you want to eat enough carbs to avoid
“zero-carb dangers” such as
mucus deficiency.
At the same time, you want to generate abundant ketones to nourish the
brain. You can achieve both by eating carbs for glucose, but also eating
short-chain fats and ketogenic amino acids to make ketones.
So let’s look at why these foods are so effective at producing ketones.
Amino Acids
The main metabolic process which converts one metabolic substrate into another is called the
citric acid cycle, tricarboxylic acid (TCA) cycle, or Krebs cycle.
The TCA cycle looks like this (blue arrows):
The passage from succinyl CoA to fumarate is where ATP is made. The cycle can be fed in several ways:
- By pyruvate which is an intermediate produced in glucose metabolism;
- By acetyl CoA which is an intermediate produced by ketones or fatty acid oxidation;
- By amino acids which can enter the TCA cycle at various points.
The green boxes show
glucogenic amino acids entering the cycle. The white boxes show
ketogenic
amino acids that are made into either acetyl CoA or acetoacetyl CoA and
thence can either leave as ketones (via HMG-CoA) or enter the cycle by
conversion of acetyl CoA to citrate.
The crucial takeaway, as far as this post is concerned, is the distribution of amino acids among green and white boxes:
- Leucine and lysine appear only in white boxes, not in green boxes. They are purely ketogenic.
- Isoleucine, tryptophan, phenylalanine, and tyrosine appear in both
green and white boxes. They can be either ketogenic or glucogenic.
- The other amino acids appear only in green boxes and are purely glucogenic.
So if the diet is rich in leucine and lysine, but poor in glucogenic amino acids, then it will be highly ketogenic.
Short-Chain Fats
Fats are made into acetyl CoA. Acetyl CoA can either enter the TCA
cycle or be converted to ketones. What decides which way it goes?
One important factor is whether the cell has enough ATP. If the cell
has plenty of ATP then it won’t allow the TCA cycle to make any more,
and the TCA cycle gets stuffed with succinyl CoA and then with all the
other intermediates in the pipeline behind it.
Once the TCA cycle is full, acetyl CoA no longer enters the cycle and instead leaves as ketones.
Long-chain fats can follow this route, but not terribly easily. They have alternatives:
- Long-chain fats can serve as structural molecules in cell membranes throughout the body.
- Long-chain fats can be stored in adipose cells.
- Long-chain fats can be burned by cells throughout the body, and transported to cells that need them.
These factors mean that you have to eat a very large amount of long-chain fats before you produce substantial ketones.
Short-chain fats (12 carbons or less in length; often called
medium-chain) are different. Short-chain fats do not appear in cell
membranes and are not stored in adipose tissue (except for a little
12-carbon fatty acids). Rather than being transported throughout the
body, they are shunted to the liver for disposal.
This means that if you eat a lot of coconut oil (which is 58%
short-chain fats), you deliver a lot of fat to the liver for disposal.
The disposal process for fat is conversion to acetyl CoA followed by
either burning in the TCA cycle or conversion to ketones.
After a big cup of coconut oil is delivered to the liver, the liver’s
ATP levels are quickly saturated. The TCA cycle is stuffed and the
liver will dispose of the coconut oil by making ketones.
It will do this whether the rest of the body needs the ketones or not.
The liver wants to get rid of the coconut oil, and it does it by making ketones whether the rest of the body wants them or not.
Summary
So we have three ways to make the diet ketogenic:
1) Make Wilder’s “ketogenic ratio” high by eating a lot of fat, very few carbs, and not too much protein.
2) Supplement with the ketogenic amino acids lysine and leucine.
3) Supplement with coconut oil or another source of short-chain fats.
If we do (2) or (3), then the diet can be ketogenic even if it has a fair number of carbs.
So now we have an arsenal of ways to generate ketones. We have to
look at diseases and diet risks to figure out which way of making the
diet ketogenic is optimal.
I’ll look at that next week.
References
[1] Owen OE et al. Brain metabolism during fasting.
J Clin Invest. 1967 Oct;46(10):1589-95.
http://pmid.us/6061736.