In a previous issue of Weightology Weekly, I wrote about insulin and how it's been unfairly demonized by many in the nutrition field.
This demonization has been based on a number of misconceptions
regarding insulin, its biological effects, and its secretion. I want to
continue clarifying these misconceptions.
MYTH: Insulin Spikes are "Bad"This demonization has been based on a number of misconceptions
regarding insulin, its biological effects, and its secretion. I want to
continue clarifying these misconceptions.
FACT: Insulin Spikes Serve a Normal & Important Physiological Function
In my previous article,
I discussed how dietary protein can cause insulin spikes just like
dietary carbohydrate, and these spikes are not related to
gluconeogenesis from the protein (i.e., the protein being converted to
sugar). I also showed how these spikes are partly responsible for the
suppression of appetite that is caused by dietary protein (due to
insulin's effects on your brain to inhibit appetite).
I want to expand on the importance of rapid insulin spikes due to
feeding, and how they are important in blood sugar regulation. To do
this, we need to discuss the phases of insulin secretion. Insulin
secretion from your pancreas comes in two phases. The first phase
happens very quickly; your pancreas senses rising glucose, and insulin
is released within 1-2 minutes of this rise in blood sugar. This
rapid-phase response is the result of your pancreas releasing stored
insulin. It is typically over within 10 minutes. This rapid-phase
response has been found to be impaired in people with impaired glucose tolerance
(people who have higher blood sugar responses to meals than normal, and
higher fasting levels of blood sugar, but who are not diabetic). This
rapid-phase response is completely absent in people with type 2
diabetes.
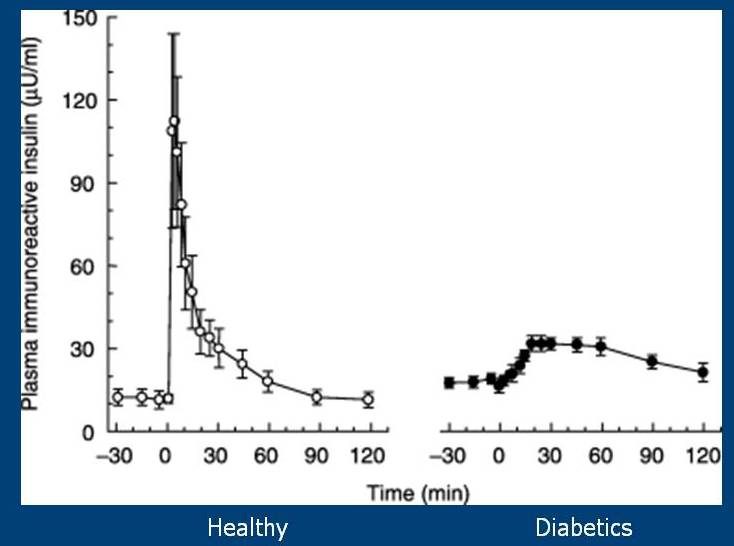
There is a second phase that continues as long as glucose is
elevated. This release of insulin is achieved by the release of stored
insulin, as well as the creation of new insulin (insulin is created from
a precursor called proinsulin). When you infuse glucose into the blood
of healthy people and type 2 diabetics, you get insulin responses that
look like this:
You can see that the diabetics completely lack the rapid phase response that is present in the healthy individuals.
There is a drug called exenatide (Byetta), which has been found to restore this rapid phase insulin response in diabetics:

Insulin
responses of type2 diabetics and healthy individuals, who have been
administered glucose intravenously. Circles represent the insulin
response of the type 2 diabetics when given a placebo. Squares represent
the insulin response of the diabetics when given exenatide. You can see
that exenatide restores the rapid phase insulin response. Black circles
represent the insulin response of healthy individuals.
responses of type2 diabetics and healthy individuals, who have been
administered glucose intravenously. Circles represent the insulin
response of the type 2 diabetics when given a placebo. Squares represent
the insulin response of the diabetics when given exenatide. You can see
that exenatide restores the rapid phase insulin response. Black circles
represent the insulin response of healthy individuals.
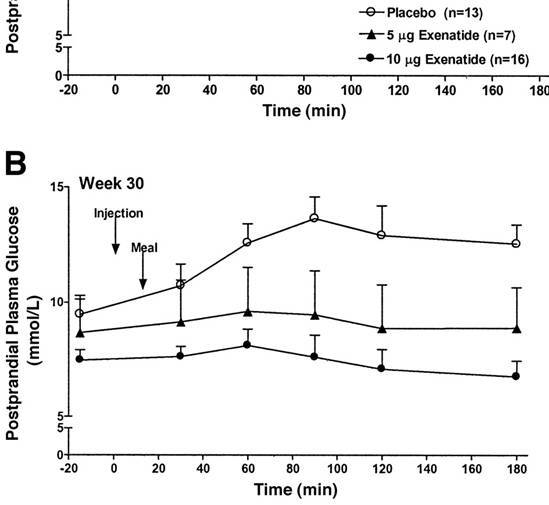
Blood
sugar response to a meal in type 2 diabetics. Circles represent
subjects on a placebo. Dark triangles and circles represent subjects on
exenatide. You can see that blood sugar remained steady in the subjects
on exenatide, but gradually increased in the subjects on the placebo.
sugar response to a meal in type 2 diabetics. Circles represent
subjects on a placebo. Dark triangles and circles represent subjects on
exenatide. You can see that blood sugar remained steady in the subjects
on exenatide, but gradually increased in the subjects on the placebo.
in response to a meal in the subjects on exenatide, but it increased
over time in the subjects on the placebo.
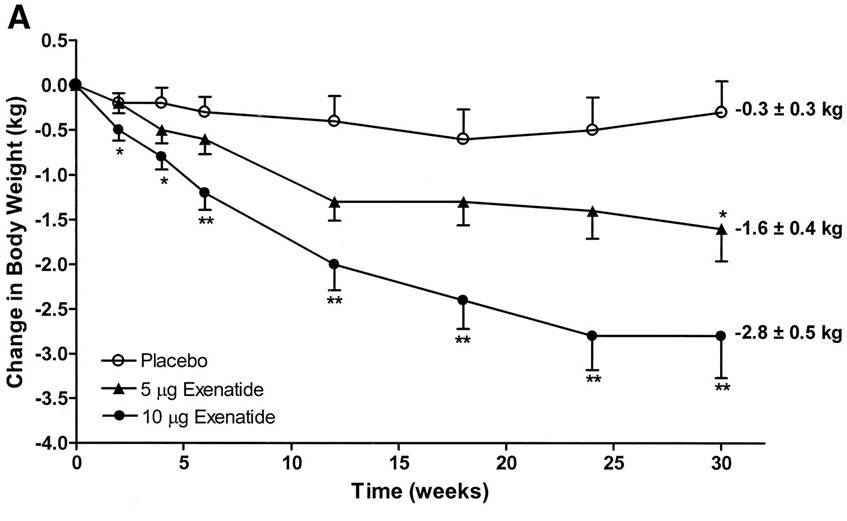
Many people like to blame obesity and weight gain on insulin, but
exenatide, which restores insulin spikes in type 2 diabetics, causes
weight loss:
Part of this weight loss is due to an improvement in satiety.
Exenatide is a drug that mimics the effects of a hormone called
glucagon-like peptide-1 (GLP-1). GLP-1 is an intestinal
insulin-stimulating hormone (known as an incretin). GLP-1 potentiates
insulin secretion, enhances the synthesis of insulin, upregulates
insulin gene expression, and inhibits glucagon (insulin's opposing
hormone) secretion. Yet Exenatide, which mimics GLP-1 and helps
stimulate insulin secretion, causes weight loss.
The fact is that rapid insulin spikes in and of themselves are not a
bad thing. Protein causes rapid insulin spikes, yet protein reduces
appetite and helps with weight loss. GLP-1 and drugs like exenatide
contribute to insulin spikes, yet they reduce appetite and cause weight
loss. The problem is that people confuse insulin spikes and blood
glucose spikes. It is well established that rapid rises and falls in blood glucose can contribute to hunger.
Because rapid rises in blood glucose also cause rapid rises in insulin,
people end up blaming insulin (and the effects of high glycemic
carbohydrates on insulin) for the problem.
MYTH: Since diabetics who inject insulin gain weight, this means that insulin is the reason for weight gain in non-diabetics
FACT: Amylin is co-secreted with insulin in non-diabetics; amylin has appetite suppressant and lipolytic effects
I would like to thank Dr. Stephan Guyenet
for this information. I had known about amylin but hadn't looked into
it in any great detail. Amylin is a hormone that is secreted by your
pancreas at the same time as insulin. Amylin decreases appetite, and also stimulates lipolysis (the breakdown of fat into fatty acids).
Type 1 diabetics do not produce amylin, and amylin secretion is impaired in type 2 diabetics. Pramlintide, a drug that mimics the effects of amylin, has been found to produce weight loss in diabetics.
This information demonstrates that the effects of insulin injection
in a diabetic cannot be compared to the effects of physiological changes
in insulin in a non-diabetic, yet many people erroneously make this
comparison as if they are similar.
MYTH: Lowering Insulin Will Improve Appetite Regulation
FACT: Insulin Is One of the Many Hormones Critical to Satiety
I already most addressed this myth in my previous article on insulin,
showing how protein stimulated insulin secretion and helped reduce
appetite, and also showing how insulin injection into the brain reduces
appetite. I again want to thank Dr. Guyenet for this information, but when you knock out the insulin receptors of a mouse's brain, the mouse will overeat and develop obesity.
MYTH: All of this information only applies to healthy people
FACT: The information applies to obesity and diabetes
On other forums, I saw people comment on my previous article and
claim that the information I provided only applied to healthy people,
and not diabetics or obese individuals. They continued to believe that
treating diabetes and obese individuals was all about insulin control.
Nothing could be further from the truth. Not only is this evident from
information mentioned earlier in this article (such as how exenatide
restores insulin spikes and improves blood sugar control and body weight
in diabetics), but it is also evident from the fact that high protein
diets have been found to help both diabetics and obese individuals,
despite the fact that protein is a powerful stimulus of insulin
secretion.
As I mentioned earlier, people seem to confuse blood glucose control
and insulin control. It is the management of blood glucose itself that
is partly responsible for the health benefits of low-glycemic
carbohydrates, or reducing carbohydrates, or increasing protein intake,
or consuming dietary fiber, or consuming fruits and vegetables, or
consuming whole foods over processed foods. It is not the control of
insulin; the control of insulin ends up being a byproduct of these other
behaviors through improvements in insulin sensitivity (how responsive
your cells are to insulin) and reductions in blood sugar swings.
Remember, insulin is not the bad guy. Click here to read part 3 of this series, where I discuss how dairy products are extremely insulinemic, yet do not promote weight gain.