Earlier
this week a paper was released to much fanfare, claiming that diets
with over 20% of energy as animal protein might be as life-threatening
as smoking.
- The Huffington Post
said, “Atkins aficionados, Paleo enthusiasts, and Dukan devotees, you
may want to reconsider what’s on your plate. While high-protein diets
have been all the rage over the last few years for their waist-whittling
goodness, a new study says they could be as bad for you as smoking.” - Scientific American
said “People who eat a high-protein diet during middle age are more
likely to die of cancer than those who eat less protein, a new study
finds.” - NPR
said, “Americans who ate a diet rich in animal protein during middle
age were significantly more likely to die from cancer and other causes.”
They added, “In an age when advocates of the Paleo Diet and other
low-carb eating plans such as Atkins talk up the virtues of protein
because of its satiating effects, expect plenty of people to be
skeptical of the new findings.” A sound prognostication!
What the Researchers Did
The article appeared in Cell Metabolism, a high-impact journalwhich likes long complex papers reporting years of work. [1] A common
strategy for getting into such journals is to piece together a great
variety of work into one article, weaving a narrative theme to unite
them. That’s what this article did, using the theme “high protein diets
may shorten lifespan” to link several relatively disconnected projects.
The NHANES Findings
The work that generated most of the buzz was an analysis of data fromthe National Health and Nutrition Examination Survey (NHANES). They
looked at a group of 6,381 NHANES respondents and found, “Respondents
aged 50–65 reporting high protein intake had a 75% increase in overall
mortality and a 4-fold increase in cancer death risk during the
following 18 years. These associations were either abolished or
attenuated if the proteins were plant derived.”
Here’s their Figure 1:
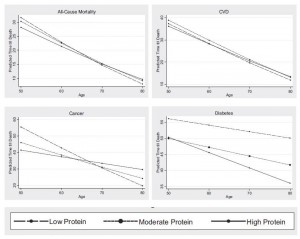
Two oddities in this result raise red flags:
- First, protein appears harmful at age 50, neutral at age 65, and
beneficial at age 80. This reversal of effects is incompatible with most
mechanisms by which protein could affect aging or disease risk. In
animal studies, we see the opposite: protein restriction extends maximum
lifespan, which means that at high ages, mortality is lower, but
increases risk of early death, which means that in middle age mortality
is higher. - Second, they report that the effect was specific to animal protein:
“[W]hen the percent calories from animal protein was controlled for, the
association between total protein and all-cause or cancer mortality was
eliminated or significantly reduced, respectively, suggesting animal
proteins are responsible for a significant portion of these
relationships. When we controlled for the effect of plant-based protein,
there was no change in the association between protein intake and
mortality, indicating that high levels of animal proteins promote
mortality.” Yet, plant and animal proteins are biologically similar.
health outcomes from protein is due to confounding factors – behaviors
or foods associated with animal protein consumption in middle age,
rather than effects caused by the protein itself.
When we look at how the analysis was performed, we find more reasons
to doubt that protein is at fault. All of this data was found using a
model which adjusted for the following covariates:
Model 1 (baseline model): Adjusted for age, sex,Adjustment for a host of health-related conditions – waist
race/ethnicity, education, waist circumference, smoking, chronic
conditions (diabetes, cancer, myocardial infarction), trying to lose
weight in the last year, diet changed in the last year, reported intake
representative of typical diet, and total calories.
circumference, diabetes, cancer, myocardian infarction, and even total
calories which is effectively a proxy for obesity – can radically
distort results, and even transform effects from positive to negative.
I’ve discussed this issue previously in The Case of the Killer Vitamins.
In practice, many factors are highly correlated. The variables being
studied – protein intake, waist circumference, total calorie intake, and
others – are beset by the problem of collinearity.
Attempting multiple regression analysis on collinear variables can
generate very peculiar results. The more the number of adjustment
factors grows, the more strange things tend to happen to data.
If they wanted us to understand whether their results are
trustworthy, authors would present raw data, and then a sensitivity
analysis that shows how introducing each covariate individually affects
the results, then showing how including combinations of two covariates
affects the results, and so forth. This would help us judge how robust
the results are to alternative methods of analysis.
Of course, authors do not do this. Instead, they ask us to trust the
analysis they have chosen to present – which is only one of billions
they could have done. (This study adjusted for 13 covariates. The NHANES
survey may have gathered data on, say, 40 variables. There are 40
choose 13, or 12 billion, possible multivariate regression analyses that
could be performed using 13 covariates on this data set. Each of the 12
billion analyses would generate different outcomes.)
Are the authors trustworthy? Unfortunately, most academics today are
not. Career and funding pressures are severe, and by and large those who
are good at gaming the funding and publishing processes have triumphed
professionally over careful, diligent truth seekers. It is much easier
to construct a narrative that will garner attention and publicity and
interest, than to carefully exclude non-robust results and publish only
those results that are solidly supported.
Frankly, I give little credence to their NHANES analysis. And,
judging by comments in the press, other epidemiologists don’t seem to
give it much credence either. From the NPR article:
But could eating meat and cheese really be as bad for you
as smoking, as the university news release describing the new Cell
Metabolism paper suggested?
Well, that may be an exaggeration, according to Dr. Frank Hu, a
researcher at the Harvard School of Public Health who studies the links
between health, diet and lifestyle.
“The harmful effects of smoking on cancer and mortality are
well-established to be substantial, while the harmful effects of red
meat consumption are modest in comparison,” Hu wrote to us in an email.
The Mouse Experiments
So let’s turn to the next part of the study, the mouse experiments:Eighteen-week-old male C57BL/6 mice were fed continuouslyThe low protein diets are really starvation diets, in terms of
for 39 days with experimental, isocaloric diets designed to provide
either a high (18%) or a low (4%–7%) amount of calories derived from
protein …
protein intake. The reason the low protein diets were sometimes 4% and
sometimes 7% was because mice will often lose weight on 4% protein diets
due to starvation (in the paper’s experiments on BALB/c mice, “the mice
had to be switched from a 4% to a 7% kcal from protein diet within the
first week in order to prevent weight loss.”). Animal control officers
do not allow experiments to continue if the mice are obviously starving.
[B]oth groups were implanted subcutaneously with 20,000 syngeneic murine melanoma cells (B16).This is an unusually small number of cells. Typically, cancer
researchers implant a million cells to create a syngeneic tumor.
Presumably they used this small number of cells in order to ensure that
some mice would not develop tumors during the 39 day experiment. As it
happened, this was a lucky (canny?) choice of cell quantity: while 10 of
10 mice on the high-protein diet developed tumors during the
experiment, only 9 of 10 mice on the low-protein diet did. If they had
used more cells, all mice on both diets would have developed tumors; if
they had used fewer cells, some mice on the high protein diet would have
failed to develop tumors. Either way, the results would appear less
damning for the high protein diet.
The outcomes:

Due to the small number of cells injected, it takes at least two weeks
before tumors are detectable in size (normally they would be visible in
ten days). They seem to be similar in size at about two weeks after
implantation.
However, when the tumors reach larger sizes, growth is impaired on
the low protein diets. A mouse weighs 20 grams, and a 2000 mm3 tumor
weighs 2 grams, or 10% of body weight – equivalent to a 15-pound tumor
in humans. Growing a tumor of this size requires building a large amount
of tissue — blood vessels, extracellular matrix, and more. The ability
to construct new tissue is constrained on a protein-starved diet, so
it’s not surprising that tumor growth is slower when the tumor is large
and protein is severely restricted.
Animal protocols generally require that mice be sacrificed when
tumors reach 2000 mm3. Extrapolating the tumor growth curves, it looks
like the mice in experiment (B) would be sacrificed 5 weeks after
implantation on the high protein diet, or 8 weeks after implantation on
the low protein diet; in experiment (G), mice on the high protein diet
would be sacrificed about 9 weeks after implantation, while mice on low
protein diets would have been sacrificed about 11 weeks after
implantation.
In other words, tumors still kill you, just a bit more slowly if you are starving yourself.
It’s important to note a couple of things. First, the word “starving”
is appropriate. 4% to 7% protein intakes are starvation levels for
mice. In a nice blog post closely relevant to this topic, Chris Masterjohn notes that a 5% protein intake completely stunts the growth of young rats:

Chris rhetorically asks: “How many of us would deliberately feed a
two-year old a diet that would cause them to stop growing altogether?”
Second, as Chris also points out in the same post, such low protein
intakes actually make cancer more likely in the context of exposure to
mutagens. For instance, aflatoxin exposure leads to cancer (or
pre-cancerous neoplasms) much more frequently in rats on low-protein
diets than in rats on high-protein diets:

In this experiment, there were two diets, 5% protein and 20% protein,
and two diet periods, one during exposure to aflatoxin and one
afterward. Rats exposed to aflatoxin while on a 5% protein diet were far
more likely to develop neoplasms than rats exposed to aflatoxin on a
higher protein diet. That is, the “20-5” rats had far fewer cancers than
the “5-5” rats, and the “20-20” rats had far fewer cancers than the
“5-20” rats. High protein for the win!
However, once the rats had neoplasms, the tumors grew more slowly on the low-protein diet. Just as the new study found.
So, if your goal is to avoid getting cancer, it is better to eat
adequate protein. If you already have cancer, or if researchers have
injected you with highly metastatic melanoma cells, you can buy yourself
slightly slower tumor growth by starving yourself of protein. In
laboratory mice, this extends lifespan a few weeks because they are not
allowed to die from cancer, but are sacrificed when tumors reach a
specific size. In humans, however, cancer death commonly follows from
cachexia, or wasting of lean tissue. A low protein diet might promote
cachexia and accelerate cancer death in humans. It is not possible to
infer from this study that there would be a clinical benefit to a low
protein diet in human cancer patients.
Other Negative Effects of Low-Protein Diets
The study noted a significant negative effect of low protein diets inolder mice. While young mice (18 weeks, equivalent to young adults)
lost only a few percent of body weight on the starvation low protein
diets, elderly mice (2 years old) wasted away on low protein diets. The
data:
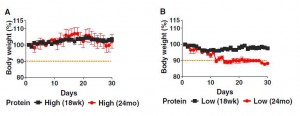
Both young and old mice managed to gain a bit of weight on the high
protein diets, and both young and old mice lost weight on the low
protein diets. The weight loss was much more severe in elderly than
young mice.
Considering that wasting away commonly precedes death in the elderly,
this is not a good sign for the low protein diets. The authors
themselves argue that this is consistent with the NHANES finding that
high protein diets become beneficial after age 65: “old but not young
mice on a low protein diet lost 10% of their weight by day 15, in
agreement with the effect of aging on turning the beneficial effects of
protein restriction on mortality into negative effects.”
However, while I think it is clear that the dramatic weight loss in
the elderly mice fed low protein is harmful, it is far from clear that
the slight weight loss of the younger mice was harmless. Though they
maintained their weight better than elderly mice, they may have been
starving as well. To actually support the NHANES survey, the researchers
should have maintained the mice on low or high protein diets for
several years, and seen which group lived longer. They did not do this.
If they had, I speculate that the high protein mice would have lived longer.
Conclusion
This is a study in the line of T. Colin Campbell and othervegetarians who have tried to show that animal protein promotes cancer
and mortality. These studies are unconvincing. They simply do not prove
the conclusions they purport to draw.
The Perfect Health Diet takes a middle ground in regard to protein:
We recommend eating about 15% protein, and argue that both high protein
and low protein diets are likely to be harmful; high protein diets by
accelerating aging or by making protein available to gut bacteria for
fermentation, producing a less beneficial gut flora and generating
nitrogenous toxins; low protein diets by starving the body of a key
nutrient needed to maintain bodily functions, especially liver, kidney,
and immune function.
Nothing in this study persuades me that those recommendations need revision.
References
[1] Levine ME et al. Low Protein Intake Is Associated with a MajorReduction in IGF-1, Cancer, and Overall Mortality in the 65 and Younger
but Not Older Population. Cell Metabolism 19, 407–417, March 4, 2014. http://www.cell.com/cell-metabolism/retrieve/pii/S155041311400062X.